Hormone & Sexual Health
Understanding Your Hormone Panel: What Testosterone, Estradiol & FSH Results Actually Mean
Dec 19, 2025

Jake Kaiser
jakesjourney.co
The Architecture of Vitality: Decoding Your Hormone Panel
When we talk about biomarkers, we usually obsess over the mechanics: blood sugar, cholesterol, inflammation. These are the "what" of your physiology. But hormones? Hormones are the "how" and the "why." They are the architects, the project managers, and the foremen of your body, sending chemical instructions to every single cell you have.
The endocrine system is a vast, interconnected web of signals that controls everything from your muscle mass and bone density to your mood and sex drive. It is super complex, and if you are dealing with a specific pathology, you absolutely need to work with an endocrinologist. However, for those of us looking to optimize our health span and ensure our bodies are receiving the right instructions for longevity and performance, there are a handful of critical markers we need to understand.
The Signal Carriers: How It Works
Before we dive into the specific markers, we need a quick mental model of the system. It all starts in the brain.
Think of your Hypothalamus and Pituitary gland as the Command Center. They monitor the body and send out "orders" via hormones like LH and FSH. These orders travel to the factories (like testes in men and ovaries in women) to turn up or down the production of Testosterone and Estrogen. These hormones then travel through the blood to the Job Sites (muscles, bones, brain, heart) to execute their work.
When you test hormones, you want to check every step of this supply chain to see how they are each working.
For Men: The Androgen Engine
For men, the focus is heavily on the HPG (Hypothalamic-Pituitary-Gonadal) axis. We are looking for robust production and efficient delivery.
1. Total Testosterone
This is the main output of your hormone factory. It measures the total amount of testosterone floating in your blood. While it's the most common test, it is only part of the story. A high total number doesn't matter if your body can't actually use it.
Standard "Normal": 250 – 916 ng/dL
Longevity Optimal: 500 – 800+ ng/dL
The Science: Consistently low levels (< 300 ng/dL) are not just about low libido; they are strongly linked to increased all-cause mortality, cardiovascular disease, and metabolic syndrome [1]. Conversely, maintaining robust levels in the upper quartiles is associated with preserved muscle mass, bone density, and cognitive function as you age.
There are people that feel great at lower testosterone levels due to their specific biology and in the end how you feel is more important than any number when it comes to testosterone. Oftentimes tracking changes is more important/useful than absolute amounts.
2. Free Testosterone
If Total T is total output Free Testosterone is the workers ready to work and in working shape. Most testosterone in your blood is bound up by proteins and biologically inactive. Free Testosterone represents the fraction (usually only 1-2%) that is unbound and actually available to enter your cells and do their work.
Standard "Normal" (Direct/Analog - e.g., LabCorp): 8.7 – 25.1 pg/mL
Standard "Normal" (Dialysis/Calculated - e.g., Quest): 35 – 155 pg/mL
Longevity Optimal: You want to be in the upper quartile of your specific lab's range.
Direct Method: > 15 pg/mL
Dialysis Method: > 100 pg/mL
The Science: This is often the more clinically relevant number. You can have "normal" total testosterone but low free testosterone, leading to deficiency symptoms (fatigue, brain fog, muscle loss). Always check which methodology your lab used before interpreting your number.
3. Estradiol (E2)
Yes, men need estrogen. In fact, it is critical for male libido, joint health, and bone density. It is produced by converting some of your testosterone into estradiol via an enzyme called aromatase.
Standard "Normal": 10 – 40 pg/mL
Longevity Optimal: 20 – 30 pg/mL
The Danger: You want the "Goldilocks" zone here. Too high can cause water retention and moodiness; too low is disastrous for bone density and sex drive.
For Women: The Cyclical Symphony
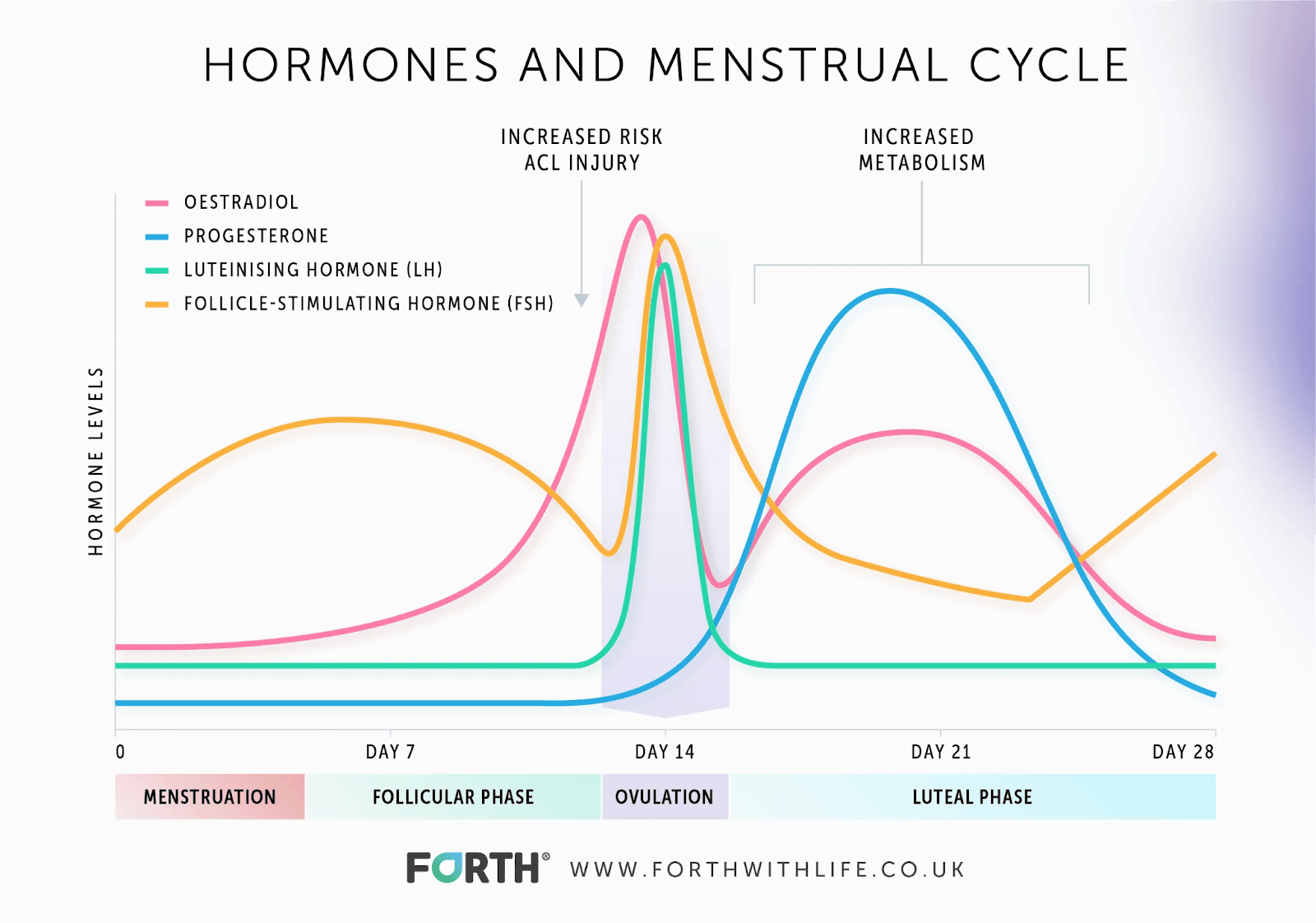
Women’s endocrinology is inherently dynamic. While men have a steady state, women have a monthly cycle (pre-menopause) or a settled state (post-menopause). Context is everything—you must know where you are in your cycle when you test.
1. Estradiol (E2)
This is the primary and most potent form of estrogen. It is the master regulator of female health, protecting the brain, heart, and bones.
Standard Ranges (Pre-Menopausal): Varies wildly by cycle phase (e.g., Follicular: 30–120 pg/mL; Ovulation Peak: 200–400+ pg/mL).
Longevity Optimal (Post-Menopausal): Without hormone therapy, levels drop near zero. In the context of longevity medicine and Hormone Replacement Therapy (HRT), many experts aim for a physiological floor to maintain bone and brain protection, often targeting levels consistent with the early follicular phase.
The Science: The rapid drop in estradiol at menopause is the primary driver for the sudden increase in cardiovascular risk and osteoporosis in women. Maintaining optimal levels is causally linked to better arterial health and cognitive resilience [2].
2. Follicle-Stimulating Hormone (FSH)
FSH is the signal from the brain to the ovaries. When the ovaries are working well, the brain sends a weak signal for lower FSH. When the ovaries start to slow down (perimenopause/menopause), the brain starts increasing this signal strength to get a response.
What it tells you: A climbing FSH is the canary in the coal mine for ovarian aging. Ideally, in a fertile state, this number is low (< 10 mIU/mL). As menopause approaches, it can skyrocket to > 40 mIU/mL.
3. Testosterone
Women produce testosterone too, and it is vital for energy, motivation, muscle tone, and libido. In fact, women have higher circulating levels of testosterone than estrogen!
Standard "Normal": 15 – 70 ng/dL
Longevity Optimal: 35 – 60 ng/dL
The Science: Keeping testosterone in the upper-normal range for women is critical for maintaining lean muscle mass (which protects metabolism) and supporting sexual wellbeing and vitality [3].
The Shared Players: Critical for Everyone
1. Sex Hormone Binding Globulin (SHBG)
Think of SHBG as the bus for your hormones. It picks up testosterone and estrogen and ferries them around the bloodstream. But here's the catch: while they are on the bus, they can't do any work. They are inactive.
Why it matters: High SHBG locks up your hormones, lowering your Free T (and Free E2). Low SHBG is often a sign of insulin resistance and fatty liver.
Optimal: You want this in the middle of the range. Too high, and you have no free hormones. Too low, and you likely have metabolic dysfunction.
2. Cortisol (Morning)
This is your primary stress hormone. It is catabolic (breaks things down). You want it high in the morning to wake you up, and low at night to let you sleep.
The Signal: Chronically elevated morning cortisol suggests a system in "fight or flight" mode, which actively suppresses your sex hormones (the body won't prioritize reproduction if it thinks you are being chased by a tiger). It is a key metric for understanding if stress is the root cause of your hormonal issues.
Your Action Plan
Hormones are not static. They fluctuate with sleep, stress, diet, and training. A single snapshot is useful, but trends are more powerful.
Test in the Morning: Hormones like testosterone and cortisol peak in the morning. Ideally test around 8:00 AM but even more importantly is to keep the time you test the same to accurately understand trends.
Women, Know Your Day: If you are pre-menopausal, test on Day 21 (mid-luteal) to see progesterone peaks, or Day 3 to see baselines. Consistency is key.
Don't Settle for "Normal": If you are a 35-year-old man with the testosterone levels of an 85-year-old, the lab report might say "normal," but your physiology will tell you otherwise.
Your hormones are the instructions your body follows every day. Make sure it's receiving the right message.
Sources
[1] https://www.acpjournals.org/doi/10.7326/M23-2781[2] https://www.jacc.org/doi/full/10.1016/j.jacc.2018.11.033 [3]https://academic.oup.com/jcem/article/104/10/4660/5556103

Jake Kaiser
jakesjourney.co